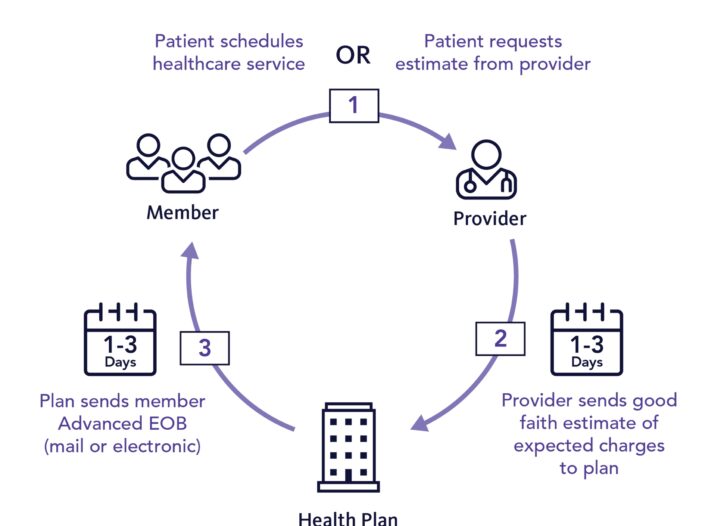
Zelis, the leading healthcare payments firm announced the results of a survey performed in July 2021 among healthcare insurers to assess their present readiness and preparation plans to meet the No Surprises Act’s criteria (NSA). The NSA aims to shield patients from unexpected medical expenditures by requiring openness and mandating members to receive an Advanced Explanation of Benefits (AEOB) for both in-network and out-of-network treatment. The majority of insurers are concerned about the NSA’s transparency rules. Meeting the AEOB standards is a problem for three-quarters of respondents. Nearly two-thirds of respondents don’t know how they’ll get the provider estimates needed for AEOBs. More than half said they were unsure if they would be able to collect the additional data needed for AEOBs.
Source: Business Wire